 Our little pumpkins are the size of plums and the Mama is sick, very very sick. I got sick while in Las Vegas and feel like I have been hit by a truck. My tonsils are the size of scallops, my body aches, and for some reason I am also throwing up. Thankfully Gabe had dinner ready when I got home last night from acupuncture, which by the way did not help my cold very much, but was "my healthy baby visit." At 12 weeks large gold needles are placed in certain places to aid in the health of the babies.
Our little pumpkins are the size of plums and the Mama is sick, very very sick. I got sick while in Las Vegas and feel like I have been hit by a truck. My tonsils are the size of scallops, my body aches, and for some reason I am also throwing up. Thankfully Gabe had dinner ready when I got home last night from acupuncture, which by the way did not help my cold very much, but was "my healthy baby visit." At 12 weeks large gold needles are placed in certain places to aid in the health of the babies. Our NT scan in on Thursday, and of course I am nervous, but if the scan comes back clear we are passing another milestone. I will post Vegas pics when I get some energy. Please keep the little pumpkins in your thoughts and prayers.
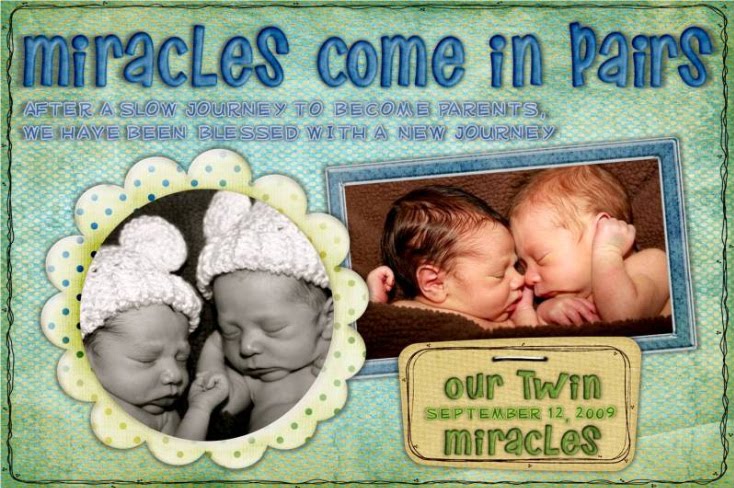
Dear Baby A & B,
We love you SO very much, we are excited to see you tomorrow. Please continue to grow strong and healthy for Mommy and Daddy. I will do my best to get well soon so that I can eat better for you and help you grow strong and healthy. We love you more and more each day. Not a day goes by that I do not feel truly blessed for the miracle that is the two of you.
All my love,
Mommy
First trimester: Check! The nausea, fatigue, mood swings, and bathroom dashes should soon fade, but (sorry!) headaches and dizziness will probably get more intense. The good news: You're about to embark on the second trimester, when mood and energy levels generally peak. As you move into the second trimester, baby shifts into the growth and maturation stage. After weeks in the critical development stage, almost all of baby's systems are fully formed. http://www.thebump.com/
The most dramatic development this week: Reflexes. Your baby's fingers will soon begin to open and close, his toes will curl, his eye muscles will clench, and his mouth will make sucking movements. In fact, if you prod your abdomen, your baby will squirm in response, although you won't be able to feel it. His intestines, which have grown so fast that they protrude into the umbilical cord, will start to move into his abdominal cavity about now, and his kidneys will begin excreting urine into his bladder. From crown to rump, your baby-to-be is just over two inches long (about the size of a lime) and weighs half an ounce.
http://www.babycenter.com/
NT Scan
Nuchal translucency screening
What is the nuchal translucency screening test?
This prenatal test (also called the NT or nuchal fold scan) can help your healthcare practitioner assess your baby's risk of having Down syndrome (DS) and some other chromosomal abnormalities as well as major congenital heart problems.The NT test uses ultrasound to measure the clear (translucent) space in the tissue at the back of your developing baby's neck. Babies with abnormalities tend to accumulate more fluid at the back of their neck during the first trimester, causing this clear space to be larger than average.The NT scan must be done when you're between 11 and 14 weeks pregnant. (The last day you can have it done is the day you turn 13 weeks and 6 days pregnant.) It's usually offered along with a blood test in what's known as first-trimester combined screening.Like other screening tests, an NT scan won't give you a diagnosis. But it can assess your baby's risk for certain problems and help you decide whether you want to have chorionic villus sampling (CVS) or amniocentesis to find out whether your baby is actually affected.The NT scan has been performed in the United States since 1995, mostly at large medical centers. Ultrasound technicians (sonographers) and doctors need special training and high-resolution ultrasound equipment to perform it correctly. They must be certified by the Fetal Medicine Foundation in London, the organization that sets the international standards and provides the software that enables a doctor to evaluate your baby's risk.Because the NT scan requires special training and equipment, it's not yet available everywhere. But the test is being done more widely as more medical personnel get trained and certified. If you're interested, ask your healthcare practitioner or genetic counselor whether it's offered in your area.
What are the advantages of first-trimester screening?
First-trimester screening lets you learn about your baby's risk for chromosomal problems relatively early in the pregnancy without subjecting yourself to the slight risk of miscarriage from an invasive test like CVS.If the risk is low, the results will offer you some reassurance. If the risk is high, you may have the opportunity to consider CVS, which will reveal whether your baby has a problem while you're still in your first trimester. (Keep in mind that CVS is usually done between 11 and 12 weeks, so to keep your options open, it's best to complete your first-trimester screening sooner rather than later.)
How can I decide which tests are right for me?
The American College of Obstetricians and Gynecologists now recommends that women of all ages be offered first- and second-trimester screening and diagnostic testing options. Your practitioner should discuss the pros and cons of various approaches with you. If you need further information, consider meeting with a genetic counselor. But ultimately, whether to test and which tests to have is a personal decision.Many women opt for screening first and then make a decision about diagnostic testing based on the initial results. Other women opt for diagnostic testing right away. (They may know that they're at high risk for a chromosomal problem or a problem that can't be detected by screening. Or they may just want to know as much as possible about their baby's condition and are willing to live with the small risk of miscarriage to find out.) Some women decide to have no screening or testing at all.
How is the NT scan done?
The sonographer first confirms your baby's gestational age by measuring him from crown to rump to see if he's about the size he should be for his age. Then she positions the sensor, called the transducer, over your abdomen so that your baby's nuchal fold area shows up on the monitor and measures the thickness of it on the screen with calipers.
How are the results computed?
Your baby's chances of having a chromosomal abnormality are determined by the nuchal fold measurement, your age, and your baby's gestational age. If you're having a first-trimester combined screening, the blood test results will also be factored in.Your age is factored in because although anyone can have a baby with a chromosomal abnormality, the risk increases as you age. For example, your likelihood of carrying a baby with Down syndrome ranges from about 1 in 1,295 at age 20 to about 1 in 82 at age 40.Researchers have measured the nuchal folds of thousands of babies between 11 and 14 weeks of pregnancy. Because a baby's nuchal fold will normally get a bit thicker with each day of gestation, they've been able to establish what an average thickness is for each day during those three weeks.They've also figured out the statistical relationship between this measurement, the baby's age, the mother's age, and the likelihood that the baby will be born with certain abnormalities. In general, the thicker the fold at a given gestational age, the higher the chance of a chromosomal problem.You may get the results right away, or you may have to wait up to ten days if the doctor has to send the data to a processing center.
What do the results mean?
You'll want to talk with your practitioner or a genetic counselor about how to interpret the results because unless you have a lot of experience with statistical analysis and evaluating medical tests, they can be confusing. And even if you're a wizard with statistics, you'll need help understanding your options.You'll get your results in the form of a ratio that expresses your baby's chances of having a chromosomal defect.For example, you may be told that your baby's chances of having Down syndrome are 1 in 30 or 1 in 4,000. A risk of 1 in 30 means that for every 30 women with this same result, one baby will have Down syndrome and 29 will not. A risk of 1 in 4,000 means that for every 4,000 women with this result, one baby will have it and 3,999 will not. The higher the second number, the lower the risk.You may also be told that your results are "normal" or "abnormal," depending on whether they are below or above a specified cutoff. For example, some tests use a cutoff of 1 in 250. So a result of 1 in 4,000 would be considered normal because the risk that there's a problem is lower than 1 in 250. A ratio of 1 in 30 would be considered abnormal because that risk is higher than 1 in 250.Remember that a normal screening result (screen negative) isn't a guarantee that your baby has normal chromosomes, but it does suggest that a problem is unlikely. Likewise, an abnormal screening result (screen positive) doesn't mean that your baby has a chromosomal problem — just that he's more likely to have one. In fact, most screen-positive babies turn out not to have a problem.(If your baby's nuchal fold measurement is above the 99th percentile for his gestational age, he's also considered to be at increased risk for major congenital heart disease, so you'll be given a special ultrasound called a fetal echocardiogram. If your baby has a heart defect, he'll need to be monitored with regular ultrasounds and delivered at a medical center equipped to handle this condition.)
How accurate is this test?
Screening tests aren't perfect. They don't detect all cases of Down syndrome, so they may identify you as being at low risk when your baby really does have Down syndrome. This is called a false negative result, and it might lead you to decide against diagnostic testing that would have revealed a problem.Conversely, screening may identify you as being at high risk when your baby is fine (a false positive). This may cause you to undergo further testing and to worry about your baby's well-being unnecessarily.How reliable a test is can be seen in its detection rate. The detection rate tells you how good the test is at identifying babies that are truly affected as being high risk. Specifically, it's the percentage of affected babies who show screen-positive results, out of all those being screened.The NT scan alone will detect about 70 to 80 percent of babies with Down syndrome (depending on which study you look at). The detection rate for the first-trimester combined screening (the NT scan plus a first-trimester blood test) ranges from 79 to 90 percent.This means that if you're carrying a baby with DS, there's a 79 to 90 percent chance that the combined screening will detect the abnormality and give you what's called a screen-positive result indicating that further testing is recommended. It also means there's a 10 to 21 percent chance that the tests will miss the DS and give you a screen-negative result.This does not mean that a screen-positive baby has a 79 to 90 percent chance of having DS. It just means that 79 to 90 percent of babies who have DS will have screening results that are suspicious enough to recommend diagnostic testing. And 10 to 21 percent of babies who have DS will be determined to be at normal risk — that is, the results will be misleading.These tests also have a 5 percent false-positive rate. A false-positive result is one that suggests there may be a problem when, in fact, there is no problem. A 5 percent false-positive rate means that 5 percent of the babies with normal chromosomes who are tested will be screen positive — that is, the test will show them to have an increased risk for Down syndrome even though they're not affected.Based on this false-positive result, their mothers may go ahead with invasive diagnostic testing that they otherwise might not have. (And they'll probably worry more, too, until they know for sure that the baby is fine.)
What if the results indicate that my baby is at high risk for a problem?
With the help of your practitioner or a genetic counselor, you'll want to decide whether the results indicate a high enough risk that you want to have CVS or amniocentesis to get a definitive diagnosis.In making your decision, you'll need to weigh your need to know about your baby's condition against the small chance that diagnostic testing could cause a miscarriage. Individual parents must decide for themselves what risks are acceptable.If you decide not to have diagnostic testing, you can get more information about your baby's health and development by following up with a detailed ultrasound at 18 to 20 weeks. This ultrasound can detect "soft markers" of chromosome disorders, such as short limbs, a bright dot in the heart, a bright bowel, and certain problems in the kidneys. It can also look for anatomical defects, such as spina bifida.








5 comments:
I hope you feel better soon. Can't wait to hear how it goes!!
Yeah!!! second trimester!!! WOO HOO!!! I hope you feel better soon mommy!! I will be praying for your scan! I;m sure all is well!
Kami
yayyyyyyyyyyyy for 12 weeks. that is SO exciting. i hope you had a great trip other than feeling crappy. i cant wait to see pics.
feel better asap! easier said than done, i know. :)
Second Tri! Way to go Mom!!!! Good luck tomorrow at the scan. I will say lots of prayers tonight for Baby A, Baby B and Mom and Dad.
Hugs!
I had every single symptom I could possible have also. I had m/s ever day until the 2nd trimester. It sucked. I hope you feel better, rest up, and good luck today. Thoughts and prayers!!
Post a Comment